COVID-19: Insights from the Johns Hopkins Center for Health Security
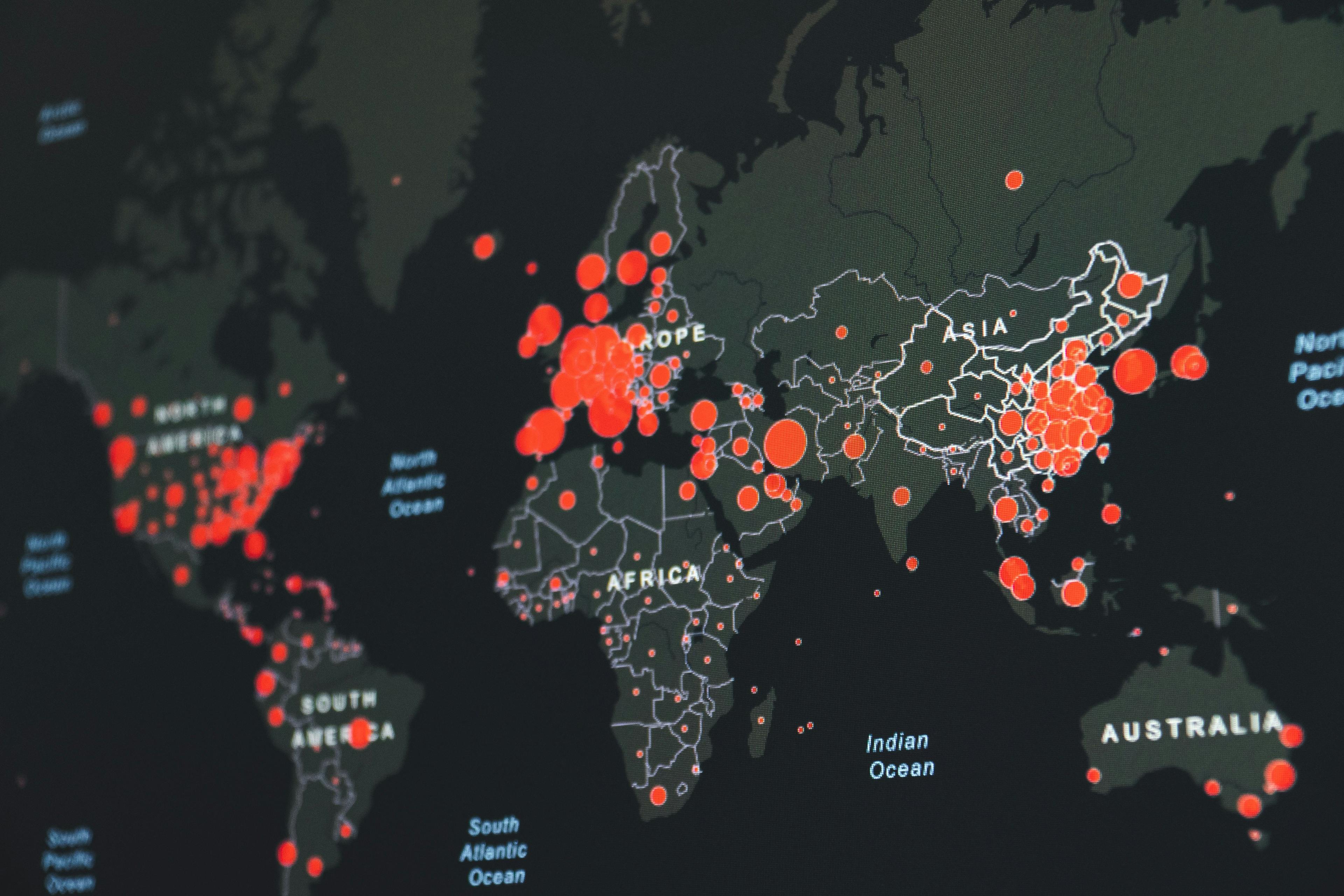
▲ Photo by Martin Sanchez on Unsplash
Following Founders Pledge’s recent webinar with the Johns Hopkins Center for Health Security (CHS), the CHS team has shared fresh insights into the COVID-19 pandemic with us, looking at the scale of the pandemic, solutions and exit strategy, and how we can prepare for future pandemics.
On the true scale & severity of the pandemic
COVID-19, resulting from SARS-CoV-2 infection, has so far caused over 2.5 million cases and 171,000 deaths globally, according to the Johns Hopkins CSSE dashboard. Reliability of case and death counts depends on a country’s ability to identify infected people through testing and contact tracing, case definitions used and frequency of reporting cases. There are likely missed cases in every country, though some may miss a greater proportion than others depending on response efforts.
At the Johns Hopkins Center for Health Security, we’ve been tracking the virus and its impact since early January. We currently don’t know the true burden of COVID-19 in the US. A small survey among pregnant women in New York found about 15% tested positive when admitted, and a serological survey in California found that between 1.8% and 5.7% of participants had SARS-CoV-2 antibodies. While emerging studies and models can be informative, each has strengths and limitations. Ways to address case underestimation include widely expanding testing and contact tracing capacity, and leveraging disease surveillance systems to capture COVID-19 cases.
The case fatality rate (CFR) and infection fatality ratio (IFR) are two ways to measure mortality. While CFR measures deaths among recognised cases, the IFR measures deaths among those infected, including mild or asymptomatic cases. We don’t know the IFR because we don’t know the proportion of undetected infections. CFR estimates vary, but a study in China estimated a range from 1.23% to 1.53%, increasing to 5.7%-7.2% for those over 60 years old. In contrast, the CFR for influenza is about 0.1%. Additionally, estimated US COVID-19 hospitalization rates are 4.6 per 100,000 population, increasing to 17.2 per 100,000 population for those over 85 years old. Given this, we know that COVID-19 is far more deadly than influenza, and capable of overwhelming health systems.
On solutions
There are several priority areas of work for addressing COVID-19 and its socioeconomic challenges.
Serological Testing Capacity
Serological tests measure antibodies to the SARS-CoV-2 virus in a person’s blood, indicating current or previous infection. Types of serological tests include rapid diagnostic tests, ELISAs, or neutralization assays. Experimental testing has been done in countries including Germany, the UK, Singapore and the US. Serology testing can be a factor that informs response measures. Government officials in various countries have cited the potential use of serology testing for “immunity certificates” to indicate a person has recovered from infection and can return to work. There are ethical and technical hurdles for using serological testing for this purpose, including the ability to manufacture tests rapidly, the accuracy of tests and appropriate and equitable use of certificates.
Contact Tracing
We are, at minimum, months away from having a safe and effective vaccine readily available, so we must rely on proven public health interventions to stop the spread of COVID-19, including contact tracing. Our Center has published a National Plan to outline comprehensive contact tracing in the US. Countries that have done extensive COVID-19 contact tracing, such as South Korea, have more effectively controlled the epidemic. Some countries have used technological approaches, including cell phone apps to support contact tracing. Use of those tools should come with substantial privacy protections. Experiences from countries that supplement in-person tracing with technology, including Iceland and New Zealand, may be applicable to the US. Since contact tracing is incredibly resource-intensive, the US Congress should provide extensive funding to state and territorial health departments. Once supported, health departments can begin recruiting contact tracers from public health fields, volunteer corps and unemployed individuals seeking work. We estimate that mobilizing a network to conduct sufficient levels of contact tracing may require recruiting approximately 100,000 contract tracers and cost $3.6B.
Vaccines
There are currently nearly 70 vaccine candidates in development, with several in phase 1 clinical trials. While a timeline of 12-18 months has been proposed for COVID-19 vaccine development, vaccines generally take at least several years to develop, test, approve and manufacture. We do not know how quickly a candidate targeting COVID-19 disease can be made, but past coronavirus vaccine development efforts have faced challenges, like antibody-dependent enhancement. Equitable vaccine allocation is an important consideration once supply is available. The World Health Organization and other stakeholders have facilitated vaccine allocation during past epidemics. Supporting their efforts to ensure equitable access, particularly to low- and middle-income countries, will be an important component in global COVID-19 response efforts.
Supporting Vulnerable Populations
Vulnerable populations at particular risk of suffering health or financial hardships due to COVID-19 include the elderly, disabled, homeless or low income, racial minorities, incarcerated, and undocumented migrants. Many people within these populations may already suffer from isolation, financial insecurity and increased health risks, which are exacerbated by the disease or the social distancing measures being implemented. Resources and support should be directed to organizations that aim to address the needs of these populations.
On the exit strategy
Social distancing, among other interventions, helps flatten the epidemic curve, reducing disease burden and health system strain. While most countries have implemented aggressive social distancing restrictions, some have favored approaches that aim to achieve widespread immunity. These approaches, however, could lead to devastating levels of disease or deaths. Additionally, it is uncertain for how long COVID-19 survivors have immunity, and therefore the theoretical benefit of the “herd immunity” approach is unknown.
Over time, as social distancing restrictions are lifted, the risk of transmission will increase to an extent. Because of this, we must take a thoughtful and careful approach to reopening of businesses, schools and every day activities. Our Center, along with others like the US government and WHO, has proposed guidelines or plans for reopening. Most agree that gradual reopening will rely on sufficient testing and contact tracing, implementing effective risk mitigation measures in public settings, and using treatments and vaccines if and when they become available. These planning efforts aim to slowly return to a more normal life over time, in ways that avoid rebounding incidence as restrictions are loosened.
Since the COVID-19 pandemic is a health and socioeconomic crisis, we believe in collaborative efforts to balance the implementation and lifting of social distancing measures with the social, health and economic needs of communities. Striking this balance in ways that foster social equity involves deliberative discussions with diverse stakeholders, like business owners, faith leaders and advocacy organizations, to inform decision-makers of a community’s needs, and find effective solutions.
On preparing for the next pandemic
Current efforts should focus on supporting response efforts. As the pandemic eventually becomes more manageable, lessons learned from this experience could inform future preparedness and response. We believe this pandemic shows the importance of maintaining a well-supported state and local public health workforce to carry out critical functions like contact tracing, surveillance, testing, vaccine or treatment administration, and helping vulnerable populations. Strengthening infrastructures that enable rapid development and manufacturing of diagnostic and serological tests are crucial, as are those for treatments and vaccines to novel emerging diseases. Finally, the pandemic has resurfaced long-standing vulnerabilities in US and global society, including ensuring support services and healthcare for migrants or low-wage workers, and enabling paid sick leave.